Freijy, T., Cribb, L., Oliver, G., et al. 2022 “Effects of a high-prebiotic diet versus probiotic supplements versus synbiotics on adult mental health: The “Gut Feelings” randomised control study”, Frontiers in Neuroscience, 16.
Effects of a high-prebiotic diet versus probiotic supplements versus synbiotics on adult mental health
What it contains
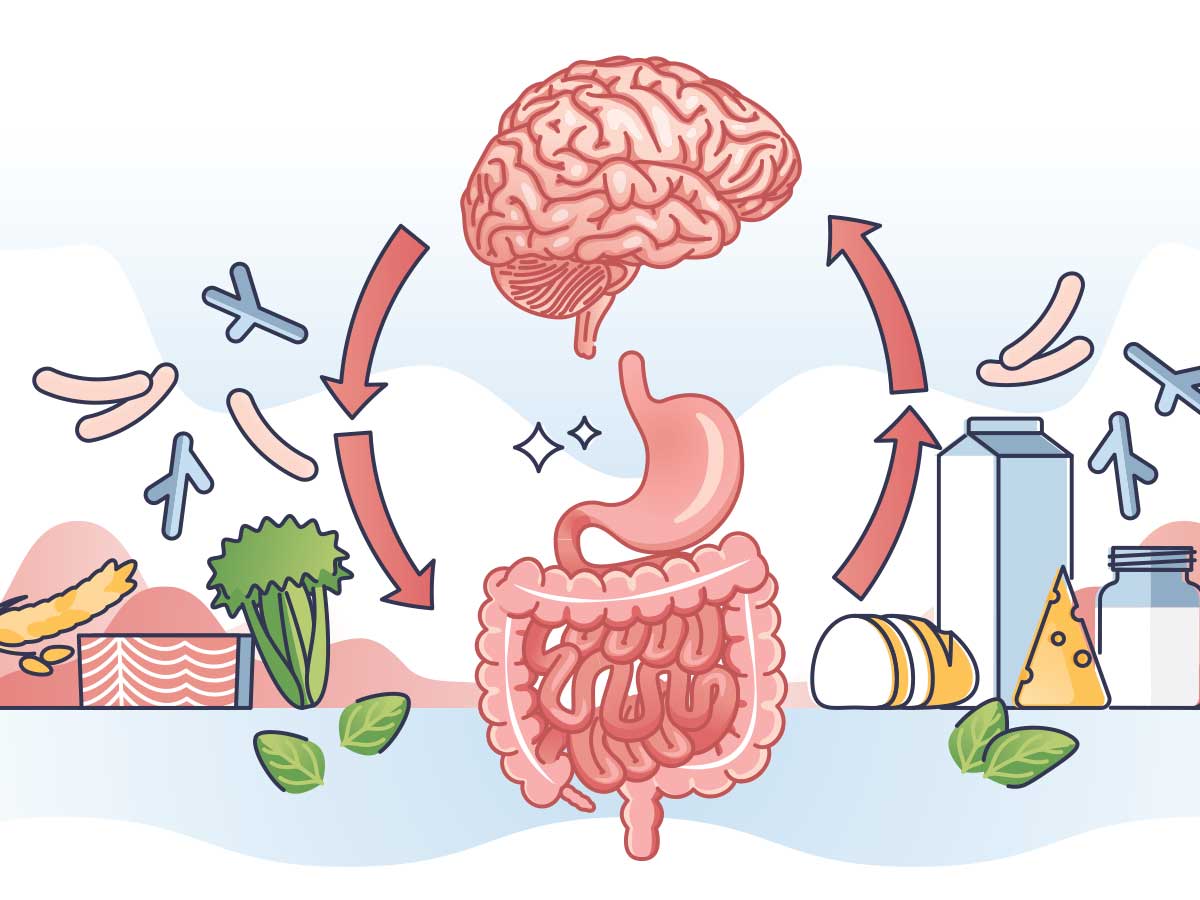
Extensive evidence suggests a communication channel exists between the gut and the brain/central nervous system. This relationship is termed the gut-brain-axis. Further that depression is associated with altered gut microbiota, due to the influence of the gut-brain-axis.
Depression in humans has been associated with bodily inflammation that arises as a result from certain bacteria inside the gut. Interestingly, the human gut microbiome is relatively stable in adulthood. However short-term changes in dietary intake can impact the composition of the gut microbiota. So, through dietary intervention, it may be possible to alter the gut bacteria, the inflammation risk and subsequent mood challenges.
One of the methods for altering the gut microbiota is through increasing the amount of prebiotics eaten per day. Common prebiotics include fructans such as fructo-oligosaccharides and also galacto-oligosaccharides. These prebiotics are a type of dietary fibre found in wholegrains, legumes, fruits, vegetables and nuts. Eating prebiotics has been shown to impact the gut and therefore the brain, via the gut-brain axis. In doing so, it may be possible to alleviate depression and depressive symptoms.
The “Gut Feelings” study
An 8-week randomised control study consisting of 119 adults, aged between 18-65. The 119 participants were identified as having moderate psychological distress and also ate a diet low In prebiotics. A dietary intake low in prebiotics is considered less than 3g of prebiotic dietary fibre per day. As part of the trial, the participants were randomly allocated to two of four treatment protocols. The first involved participants eating their regular diet in addition to consuming a probiotic supplement, called the Probiotic Group. The probiotic supplement contained 12 billion colony forming units per capsule, with various Bifidobacterium and Lactobacillus species.
The second involved eating a high-prebiotic diet with a placebo supplement, called the Prebiotic Diet Group. The high-prebiotic diet followed in this study was an adaptation of Monash University’s Department of Gastroenterology High Fibre, High-Prebiotic Diet. This including seven or more servings of prebiotic-rich foods per day.
The third was a high-prebiotic diet and a probiotic supplement, called the Synbiotic Group and the final treatment was the Placebo Group with a placebo supplement and their usual diet. The participants were assessed at the commencement of the trial and also at 8 weeks, upon completion of the consumption phase. They were assessed for mood disturbances including anxiety, depression, stress, sleep and general wellbeing measures.
Summary
The increase in prebiotic consumption resulted in the participants in the Prebiotic Groups, consuming higher levels of fructans, B-glucan, resistant starch and polyphenols. They also had an improved total dietary score with the increase in plant foods and dietary fibre.
Eating a diet that is high in prebiotics may improve mood, anxiety, stress and sleep; in adults with moderate psychological challenges, and also that currently consume a diet low in prebiotics. The combined high-prebiotic diet with a probiotic supplement did not produce a more favourable outcome over the Prebiotic Group alone. Further, the Probiotic Group did not have a beneficial effect on mental health outcomes.





